Percutaneous Coronary Intervention (PCI)

treatment
table of contents
Coronary artery disease
Terminology
Where is it done?
PCI procedures may include
Primary PCI
What is stent placement?
Reasons for the procedure
Risks of the procedure
Before the procedure
After the procedure
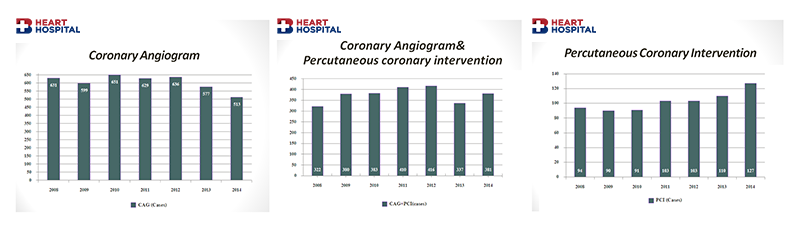
PERCUTANEOUS CORONARY INTERVENTION (PCI) AT BANGKOK HEART HOSPITAL
Coronary artery disease
Coronary artery disease (CAD) is the narrowing of the coronary arteries (the blood vessels that supply oxygen and nutrients to the heart muscle), caused by a buildup of fatty material within the walls of the arteries. This process causes the inside of the arteries to become narrowed, limiting the supply of oxygen-rich blood to the heart muscle. To better understand how coronary artery disease affects the heart, a review of basic heart anatomy and function is helpful.
The heart is basically a pump. The heart is made up of specialized muscle tissue, called the myocardium. The heart’s primary function is to pump blood throughout the body, so that the body’s tissues can receive oxygen and nutrients. Like any pump, the heart requires fuel in order to work. The myocardium requires oxygen and nutrients, just like any other tissue in the body. The blood that passes through the heart’s chambers is only passing through on its trip to the rest of the body. This blood does not give oxygen and nutrients to the myocardium. The myocardium receives its oxygen and nutrients from the coronary arteries, which lie on the outside of the heart.
Terminology
(PCI) – Percutaneous coronary intervention
(PTCA) – Percutaneous transluminal coronary angioplasty, formerly known as balloon angioplasty
Percutaneous coronary intervention (PCI) is one of the two coronary revascularization techniques currently used in the treatment of coronary artery disease, the other being coronary artery bypass grafting (CABG).
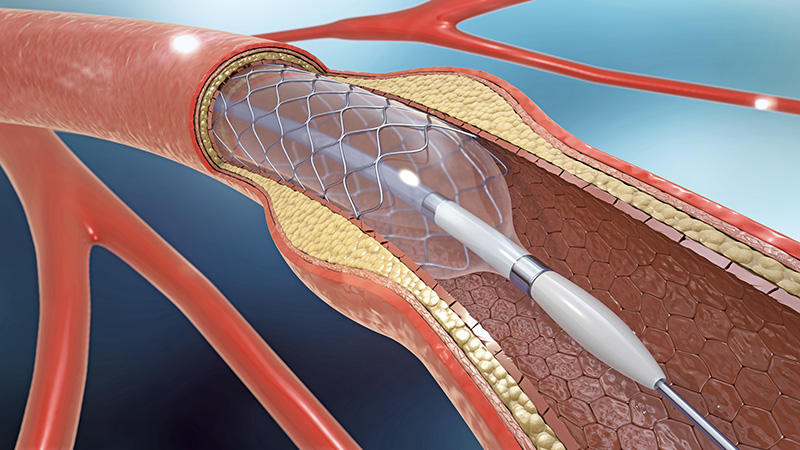
PCI involves non-surgical widening of the coronary artery, using a balloon catheter to dilate the artery from within. A metallic stent is usually placed in the artery after dilatation. Antiplatelet agents are also used to decrease thrombosis and restenosis. Stents may be either bare metal or drug-eluting or Bioresorbable stent

Where is it done?
PCI is done in cardiac catheterization laboratory like coronary angiogram, electrophysiology study and ablation and devices implantation.
PCI procedures may include
- Start with coronary angiogram
- Coronary angioplasty (balloon dilatation)
- Coronary stenting
- Coronary atherectomy
- Coronary Intravascular ultrasound
- Measuring Fractional Flow Reserve
Once the doctor has review the coronary angiogram result and has recommended the PCI appears to be the best treatment option for you and has discuss with you and the family and if you and the family agree with, then the PCI procedure will be performed.
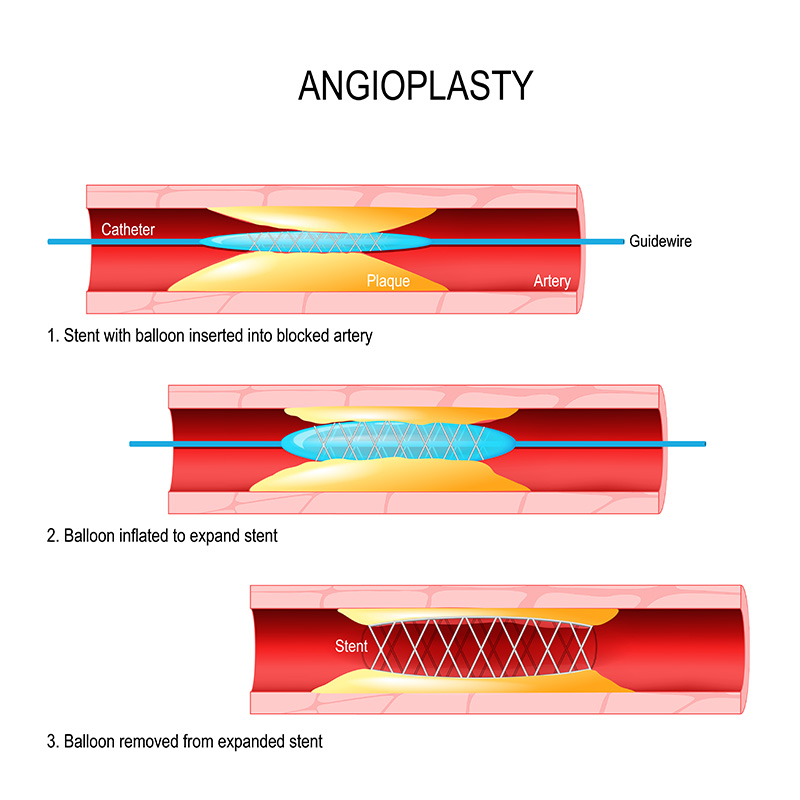
- PTCA Percutaneous transluminal coronary angiography) is performed to open blocked coronary arteries caused by cholesterol plaque and blood clot and to restore arterial blood flow to the heart tissue without open-heart surgery. Using a guide wire, a special catheter (long hollow tube) is inserted into the coronary artery and past the blockage. When the catheter is in place, the tiny balloon which is mounted onto the distal end of the catheter was inflated. The inflation of the balloon compresses the fatty tissue in the artery and makes a larger opening inside the artery to improved blood flow. The use of fluoroscopy (a special type of X-ray, similar to an X-ray “movie”) assists the doctor in the location of blockages in the coronary arteries as the contrast dye moves through the arteries.
- IVUS (intravascular ultrasound) a technique that uses the catheter with a tiny transducer that sends out sound waves to create images of the blood vessel wall. The use of IVUS provides direct visualization and measurement of the inside of the blood vessels and may assist the doctor in selecting the appropriate size of balloons and/or stents. IVUS can be used to ensure that a stent, if used, is properly opened, or to evaluate the use of other angioplasty instruments.
- FFR (Fractional flow reserve) technique called fractional flow reserve assessment is of used during a catheterization to assist in determining the significance of a moderate coronary narrowing. The technique involves placing a pressure-transducer wire across the narrowing, and after a brief infusion of medication, measuring the pressure change in the coronary artery. This may assist the doctor in deciding whether PCI or stenting is appropriate.
- Coronary atherectomy The doctor may determine that another type of procedure is necessary. This may include the use of atherectomy call rotablater, which uses high speed spinning tip catheter to grind the plaque and calcium at the site of the narrowing of the artery.
Primary PCI
If you have a heart attack the type called STEMI (ST Elevation Myocardial Infarction), it is recommended that you should undergo emergency PCI within 90-120 minutes after you are diagnosed of having this condition.
What is stent placement?
Coronary stents are now almost universally used in PCI procedures, often following balloon angioplasty, which opens the narrowed artery and facilitates stent placement. A stent is a tiny, expandable metal coil that is inserted into the newly-opened area of the artery to help keep the artery from narrowing or closing again. Once the stent has been placed, tissue will begin to form over it within a few days after the procedure. The stent will be completely covered by tissue within a month or so. It is necessary to take medications, such as aspirin, clopidogrel (Plavix), prasugrel (Effient), or ticagrelor (Brilinta), which decrease the “stickiness” of platelets (special blood cells that clump together to stop bleeding), in order to prevent blood clots from forming inside the stent. Your doctor will provide specific instructions regarding which medications need to be taken and for how long. Newer stents (drug-eluting stents, or DES) are coated with medication to prevent the formation of scar tissue inside the stent. These drug-eluting stents release medication within the blood vessel itself. This medication inhibits the overgrowth of tissue that can occur within the stent. The effect of this medication is to deter the narrowing of the newly stented blood vessel. Because stents can become blocked, it is important for you to talk with your doctor about what you need to do if you experience chest pain after a stent placement. If scar tissue does form inside the stent, a repeat procedure may be performed, either with balloon angioplasty or with a second stent.
Reasons for the procedure
PCI is performed to restore coronary artery blood flow when the narrowed artery is in a location that can be reached in this manner. Not all coronary artery disease can be treated with PCI. Your doctor will decide the best treatment of your CAD based on your individual circumstances. There may be other reasons for your doctor to recommend a PCI.
Risks of the procedure
- Bleeding at the catheter insertion site (usually the groin, or the wrist)
- Blood clot or damage to the blood vessel at the insertion site
- Blood clot within the vessel treated by PCI or stent
- Infection at the catheter insertion site
- Cardiac dysrhythmias or arrhythmias (abnormal heart rhythms)
- Myocardial infarction
- Stroke
- Chest pain or discomfort
- Rupture of the coronary artery, requiring open-heart surgery
- Risk associate with pregnancy, dye allergy and other specific medical conditions.
- Discuss with your doctor about risk and benefit of this procedure in your case.
Before the procedure
- Your doctor will explain the procedure to you and offer you the opportunity to ask any questions that you might have about the procedure.
- You will be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if something is not clear.
- Notify your doctor if you have ever had a reaction to any contrast dye, latex, tape, any medications
- You should notify your doctor. If you are pregnant or suspect that you may be pregnant.
- Notify your doctor of all medications (prescription and over-the-counter) and herbal supplements that you are taking.
- Notify your doctor if you have a history of bleeding disorders or taking medication effecting bleeding or blood clotting. It may be necessary for you to stop some of these medications prior to the procedure.
- Based on your medical condition, your doctor may request other specific preparation.
- You will need to fast for a certain period of time prior to the procedure.
After the procedure
- You will remain flat in bed for 4-6 hours after the procedure to prevent bleeding from the catheter entry site (much less time if the entry site is from the wrist or arm). If your doctor placed a closure device, your bed rest may be of shorter duration. Your affected leg or arm should not be moved or bent aggressively.
- You will most likely spend the night in the hospital after your procedure. Depending on your condition and the results of your procedure, your stay may be longer.
At home
- Once at home, you should monitor the catheter insertion site for bleeding, unusual pain, or swelling. A small or medium size bruise is normal. If you notice a constant or large amount of blood at the catheter entry site, notify your doctor.
- If your doctor used a closure device for your catheter insertion site, you will be given specific information regarding the type of closure device that was used and how to take care of the insertion site.
- There will be a small knot, or lump, under the skin, where the catheter insertion site was. This is normal. The knot or lump should gradually disappear over a few weeks.
- Some patient may develop purple skin of various size over the catheter insertion site which should gradually disappear in a few weeks.
- Your doctor will give you specific bathing instructions. You may be advised not to participate in any strenuous activities for few days.
- Your doctor will instruct you about when you can return to work and resume normal activities.
- Notify your doctor to report any of the following:
- Fever and/or chills
- Increased pain, redness, swelling, or bleeding or other drainage from the insertion site
- Coolness, numbness and/or tingling, or other changes in the affected extremity
- Chest pain/pressure, nausea and/or vomiting, profuse sweating, dizziness, and/or fainting.
PERCUTANEOUS CORONARY INTERVENTION (PCI) AT BANGKOK HEART HOSPITAL