Cardiac Electrophysiology (CEP)

diagnosis
table of contents
What is an electrophysiology study (EP test or EP study or EPS)
What are the information obtained from EP Study?
What is catheter ablation?
Where is the EP study performed?
Risks of the procedure
How do I prepare for EPS?
What happens during EPS?
What happens after EPS?
How can I learn more about EPS?
What happens after I get home?
Call your doctor's office if
What is an electrophysiology study (EP test or EP study or EPS)
An electrophysiology study (EP test or EP study or EPS) is an invasive procedure to help assess the electrical activity and electrical conduction pathways of the heart. It is the study to investigate the cause, location of origin, and best treatment for various abnormal heart rhythms. (Please see arrhythmia).
Your doctor usually will use other non-invasive tests such as a standard EKG, Holter monitor, event recorder, stress test, echocardiogram to help the diagnosis the arrhythmia before recommending the EP study.
What are the information obtained from EP Study?
- Where an arrhythmia is coming from.
- How well certain medicines work to treat your arrhythmia.
- If they should treat a problem by destroying the place inside your heart that is causing the abnormal electrical signal. This procedure is called catheter ablation.
- If a pacemaker orimplantable cardioverter defibrillator (ICD) might help you.
- If you are at risk for heart problems such asfainting or sudden cardiac death due tocardiac arrest (when your heart stops beating).
- To evaluate symptoms such as dizziness, fainting, weakness, palpitation, or others for a rhythm problem when other noninvasive tests have been inconclusive
- There may be other reasons for your doctor to recommend an electrophysiological study
What is catheter ablation?
- During an ablation, high-frequency electrical energy is delivered through a catheter to a small area of tissue inside the heart that causes the abnormal heart rhythm. This energy “disconnects” the pathway of the abnormal rhythm. Ablation is used to treat most PSVTs, atrial flutter, atrial fibrillation, and some atrial and ventricular tachycardia. Ablation may be combined with other procedures to achieve optimal treatment.
Where is the EP study performed?
The EP Study is performed in an EP laboratory which is a cardiac catheterization laboratory with additional equipment for EP study.
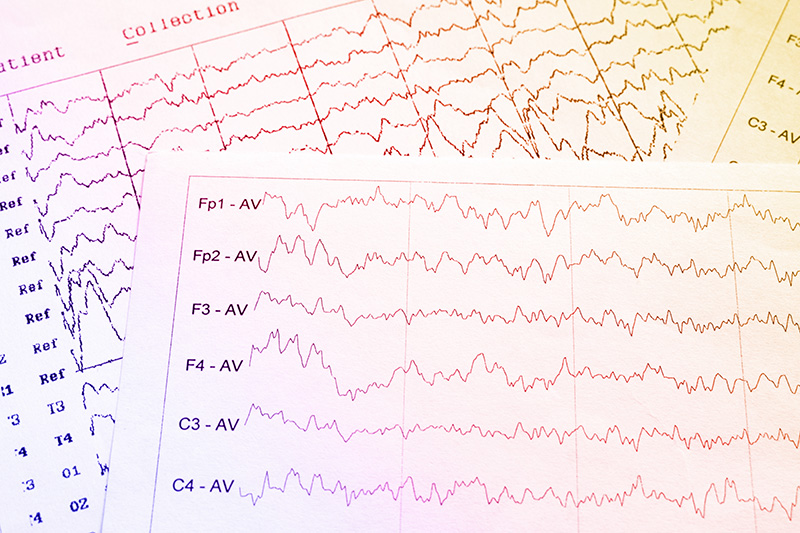
An electrophysiology study (EP study) requires insertion of more than one electrode catheters and computers to create electrocardiogram (EKG) tracings and mapping the electrical activities from inside your heart.
Risks of the procedure
As with most procedures done on your heart and blood vessels, an EP test has some risks. Major complications are rare, though. Potential risks and complications include:
- Bleeding from the catheter insertion site(s)
- Damage to the vessels for catheterization
- Infection of the catheter site(s)
- Perforation of the heart and cardiac tamponade
- Heart attack
- Stroke
- Radiation exposure risk
- Induction of significant arrhythmias
- Risk associate with pregnancy, dye or medications allergy and risk from other specific conditions.
How do I prepare for EPS?
- Don’t eat or drink anything for 6 to 8 hours before the test.
- Tell your doctor about any medicines you take, including over-the-counter medicines, herbs and vitamins. You may be asked not to take them before EPS. Don’t stop taking your regular medicine until your doctor tells you to.
- Have someone drive you to your appointment and take you home.
- If you usually wear a hearing aid, wear it during your procedure. If you wear glasses, bring them to your appointment.
What happens during EPS?
- An IV (intravenous line) is placed in your arm.
- Your nurse will clean and shave the part of your body where the doctor will be working. This is usually in the groin but may be the arm or neck.
- You will receive sedation for relaxing or moderate sedation for some procedure
- A local anesthetic will be given to make the sheath insertion area numb. A small straw-sized tube called a sheath will be inserted into your artery or vein. The doctor will gently guide several specialized EP catheters into your blood vessel through the sheath and advance them to your heart. A video screen will show the position of the catheters. You may feel some pressure in the area where the sheath was inserted, but you shouldn’t feel any pain.
- Your doctor will send small electric pulses through the catheters to make your heart beat at different speeds. You may feel your heart beat stronger or faster.
- Electrical signals produced by your heart will be picked up by the special catheters and recorded. This is called cardiac mapping and allows the doctor to locate where arrhythmias are coming from.
- When it is done, your doctor will remove the catheters. Your nurse will put pressure on the puncture site to stop any bleeding.
- EPS usually last 2 to 6 hours.
If the type and location of the arrhythmia is identified and an appropriate therapy decided, cardiac ablation or insertion of a pacemaker or ICD may be performed during or immediately after the EPS. All of these treatment probability should be discussed with your doctor before the procedure.
What happens after EPS?
- You’ll be moved to a recovery room where you should rest quietly for 1 to 4 hours.
- Be sure to keep the arm or leg used for the test straight.
- Your nurse will check on you periodically to see if there is bleeding or swelling at the puncture site.
- Your doctor will talk to you about your test results after the sedative wears off, although there may be a period of time that you may not remember that discussion well despite that you appear to be widely awake. Before you leave, you’ll be told what to do at home.
How can I learn more about EPS?
Talk with your doctor. Here are some good questions to ask:
- Are there medicines that I can use to control my abnormal heartbeats?
- Will I need a pacemaker or implantable cardioverter defibrillator (ICD) now or in the future?
- What caused my irregular heartbeat?
- Am I at risk of serious heart rhythm problems in the future?
What happens after I get home?
- Follow the instructions your nurse or doctor gave you, including taking any new medicines that were prescribed.
- Time to resume various activities depend on type of procedure that was done in addition to the EP test.
- The puncture site may be sore for several days. A small bruise at the puncture site is normal.
Call your doctor's office if
- You notice bleeding, new bruising or swelling at the catheter site
- You develop increasing pain or discomfort at the catheter site
- You have signs of infection, such as redness, drainage or fever
- There’s a change in temperature or color of the leg or arm that was used for the procedure
- You feel faint or weak.
- You develop chest pain or shortness of breath
- The puncture site begins to swell or fluids begin to come from it
- If the catheter site is actively bleeding or begins swelling, apply pressure to the site and contact emergency medical services.

