Aortic Aneurysm

treatment
table of contents
How does an aortic aneurysm occur?
Possible causes of Aortic aneurysm
Indication for repair
Treatment
Alternative treatment to surgical or endovascular repair
What will happen if I choose not to have the operation?
What does the procedure involve?
Open abdominal surgery repair
Endovascular repair for aortic aneurysm (or aortic dissection)
How does an aortic aneurysm occur?
The aorta carries blood from the heart to the rest of the body. The aorta starts from the top of left ventricle (the heart pumping chamber) ascending for short distant then arches in the upper portion of the chest and down inside the chest to reach the abdomen, then divides into legs arteries. Part of aorta inside of the chest are called
- Ascending aorta,
- Arch of aorta,
- Descending aorta.
Portion in the abdominal cavity is called abdominal aorta. An aneurysm is an enlargement (or dilatation) of the aorta and it is usually due to aortic wall weakening creates by a process call atherosclerosis.
The causes of atherosclerosis are history of smoking, high blood pressure, high cholesterol levels, diabetes mellitus and genetics factors.
The abdominal aorta is the most common site for the aneurysm to develop. Patients may have been unaware that they have an aneurysm because it often does not cause any symptoms. However, if the aneurysm is too big then the wall becomes thin and the aneurysm can tear/break/rupture. This is usually fatal. As the aneurysm gets bigger, the risk of rupture increases. Once the aneurysm reaches a size greater than 5.5 centimeters in diameter or a rapid enlarging aneurysm, a surgical (or endovascular) repair the condition is recommended as the risks of rupture are greater than the risk associated with the repair procedures.
Possible causes of Aortic aneurysm
- Smoking
- Connective tissue disorder
- High blood pressure
- Infection
- High cholesterol
- Inflammation
- Diabetes mellitus
- Presence of bicuspid aortic valve
- Genetic
Indication for repair
- Prevent risk of rupture
- When risk of rupture out weights risk of surgery
- Relieve symptoms
- Emergency bleeding
- Size of aneurysm greater than 5 cm
- Source of emboli
- Growth of aneurysm greater than 0.5 cm/year

Treatment
- Open surgery repair
- Endovascular repair
Alternative treatment to surgical or endovascular repair
- You can choose to leave the aneurysm alone, but the risk of rupture and sudden death remain.
- Lifestyle and medication changes may slow down the aneurysm enlarging but will not reverse the damage that is already done.
What will happen if I choose not to have the operation?
Aneurysms will get bigger with time. The larger they are, the weaker the wall becomes and therefore the greater the risk of the aneurysm tears or ruptures. If this were to occur, the chances of survival are poor, as on average only 1 in 4 patients with a ruptured aneurysm survives.
What does the procedure involve?
Your procedure will involve a general anesthetic and your anesthetist will discuss this with you prior to the operation.
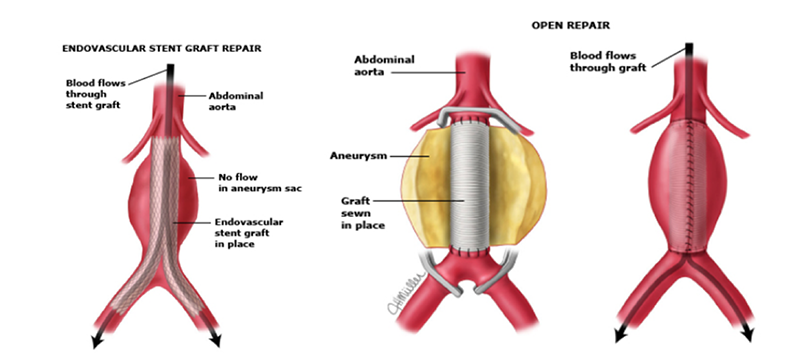
In the open surgery repair: The surgeon makes a long cut in your abdomen. The aorta is clamped and then opened. Small arteries may need to be stitched up and then an artificial graft is sewn into place. The abdominal wall and the skin are then closed.
In endovascular repair: A catheter is insert into the groin artery. A pre arrange stent was then place over the aneurysm segment. The stent will become a new aortic wall.
Open abdominal surgery repair
What risks or complications may occur?
We make every effort to reduce complication. This may include prescribing medication to reduce the risk of complications. However, every procedure has risks and potential complications. Each patient is different and the complication also depend on the complexity of the aneurysm of that patient. Those most relevant to this operation are listed below. Please discuss them with your doctor if there is anything you do not understand.
The risks and complications fall into three categories:
Complications of anesthesia:
Your anesthetist will be able to discuss the risks of anesthesia with you.
General complications of any operation:
- Pain, which occurs with every operation. Effort will be made to minimize the pain. You will be given medication to control the pain and it is important that you take it as instructed so you can move about and cough freely.
- Bleeding, which can occur either during or after the operation. This usually necessitates a blood transfusion and occasionally another operation is necessary.
- Infection in your surgical wound. You may need antibiotics or occasionally another operation to treat your infection.
- Blood clots in the legs (leg vein thrombosis), which can occasionally move through the bloodstream to the lungs causing breathing difficulties (pulmonary emboli). You will be encouraged to get out of bed soon after your operation and you may be given injections to reduce the risks of blood clots.
Specific Risks Specific complications of this operation:
- Death can occur as a result of this major operation (Risk: overall 1 in 20 but lower for fitter patients).
- Impotence is a common problem after this operation (Risk: 4 in 5 male patients).
- Problems with the graft or stitches can lead to an infected graft (Risk: 1 in 50), a small leak into a blood clot called a pseudoaneurysm (Risk 1:33) or an abnormal attachment between the aorta and the bowel called an aorto-enteric fistula (Risk: 1 in 50).
- Abdominal pain and bleeding resulting in a narrowed bowel caused by insufficient blood supply to the bowel (ischemic colitis). Occasionally another operation may be required to correct this (Risk: 1 in 50).
- Blockage of the leg arteries caused by blood clot (distal embolism). This can normally be corrected but may require another smaller procedure called an embolectomy. Occasionally this problem cannot be corrected and may lead to loss of part of the lower limb (Risk: 1 in 50).
What can I do to help operation be successful?
Lifestyle changes
If you smoke, try to stop smoking now. There is strong evidence that stopping smoking several weeks or more before a general anesthetic reduces your chances of complications.
Medications
- You should continue your normal medications. However, if you are on Warfarin (or any other blood thinning medication) you will need to stop taking it before your operation. Make sure your surgeon is aware you are on Warfarin and follow advice about stopping it.
- If you are on hormone replacement therapy or the oral contraceptive pill, it may be advisable to stop these medications before your operation. If stopping the contraceptive pill, make sure you use an alternative form of contraception.
- Important Note: Before stopping any medication, you should always ask the advice of your surgeon or doctor.
How soon will I recover?
In hospital
- After the operation you will be transferred to the Intensive care or high dependency unit for routine postoperative monitoring. Most patients are transferred back to the ward within 24 hours following the operation.
- You will gradually improve over the next few days and will be encouraged to get out of bed mobilized by the physiotherapist.
- Usually in less than a week following the operation, patients are beginning to eat a normal diet and will be mobile. Most patients stay for ten days before being discharged from the hospital.
- If you are worried about anything, whether in hospital or at home, ask a member of the healthcare team. They should be able to reassure or identify and treat any complications.
Return to normal activities
- You will be advised when to return to work depending on the extent of surgery and your type of work. Most patients will require about three months off work for this sort of operation.
- As this operation involves the muscles of the abdominal wall you should avoid manual work at first, particularly heavy lifting.
- Do not drive until you are confident about controlling your vehicle in an emergency and always check with your insurance company first.
Full Recovery
Most patients make a full recovery, though it may take up to three months to feel back to normal.
Endovascular repair for aortic aneurysm (or aortic dissection)
-
(EVAR) Endovascular aortic/aneurysm repair
-
(TEVAR) Thoracic endovascular aortic/aneurysm repair
What is EVAR OR TEVAR
EVAR or TEVAR is a minimally-invasive (without a large abdominal incision) procedure performed to repair an abdominal aortic aneurysm.
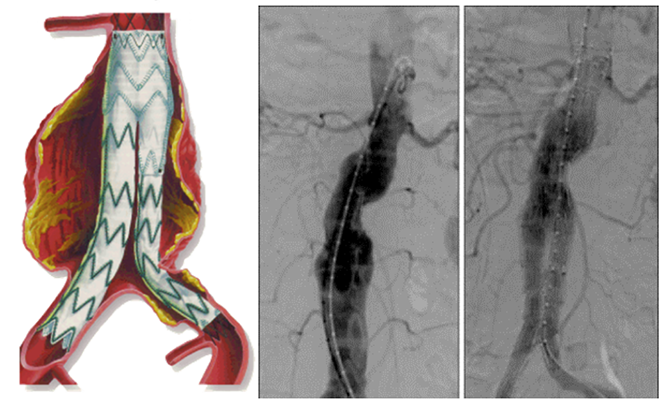
The procedure involves the placement of an expandable stent graft within the aorta to treat aortic disease without operating directly on the aorta.
Technological advancement and more operator experience is likely to prove that this technique is safer than open repair and patient anatomy limitation will be less.
Pre-procedure evaluation
Pre-procedure evaluation include CT scan for detail information of the anatomy of the aorta that include the area of abnormality, branches vessels, femoral arteries.
Procedure
The procedure is carried out in a sterile environment under x-ray fluoroscopic guidance.
- It may be performed in an operation room, radiologic department or in catheterization laboratory.
- It is usually carried out by a vascular surgeon, and an interventional radiologist, or interventional cardiologist.
- The procedure can be performed under general, regional (spinal or epidural) or even local anesthesia.
- The usual approach is from the femoral or iliac arteries where a cut down will be made or percutaneous technique is used.
- With the use of special endovascular instruments, along with X-ray images for guidance, a stent-graft will be inserted through the femoral artery and advanced up into the aorta to the site of the aneurysm.
- A stent-graft is a long cylinder-like tube made of a thin metal framework (stent), while the graft portion is made of various materials such as Dacron or polytetrafluoroethylene (PTFE) and may cover the stent. The stent helps to hold the graft in place.
- The stent-graft is inserted into the aorta in a collapsed position and placed at the aneurysm site. Once in place, the stent-graft will be expanded (in a spring-like fashion), attaching to the wall of the aorta to support the wall of the aorta. The aneurysm will eventually shrink down onto the stent-graft.
Risks of the procedure
- Damage to surrounding blood vessels, organs, or other structures by instruments
- Kidney damage
- Limb ischemia (loss of blood flow to leg/feet) from clots
- Groin wound infection
- Groin hematoma (large blood-filled bruise)
- Bleeding
- Endoleak (continual leaking of blood out of the graft and into the aneurysm sac with potential rupture)
- Spinal cord injury
There may be other risks depending on your specific medical condition such as allergic to or sensitive to medications, contrast dyes, iodine, or latex. Be sure to discuss any concerns with your doctor prior to the procedure.
What can I do to help operation be successful?
Lifestyle changes
If you smoke, try to stop smoking now. There is strong evidence that stopping smoking several weeks or more before a general anesthetic reduces your chances of complications.
Medications
- You should continue your normal medications. However, if you are on Warfarin (or any other blood thinning medication) you will need to stop taking it before your operation. Make sure your surgeon is aware you are on Warfarin and follow advice about stopping it.
- If you are on hormone replacement therapy or the oral contraceptive pill, it may be advisable to stop these medications before your operation. If stopping the contraceptive pill, make sure you use an alternative form of contraception.
- Important Note: Before stopping any medication, you should always ask the advice of your surgeon or doctor.
How soon will I recover?
The EVAR and TEVAR is only a minimal invasive procedure that does not involve large open incision. Compared to open surgery, you should recover more quickly and will be able to go home in about 3 to 5 days. There is also less pain and less complication.
Since individual patient is different, sometime by several factors, the doctor will determine which surgical intervention is most appropriate, either open repair or EVAR.
You have been found to have an aneurysm of your aorta. Your surgeon has recommended the procedure to treat this condition. However, the decision is yours as to whether to proceed with an operation or not. If you have any questions that are not answered by this document, you should ask your surgeon or any member of the healthcare team.